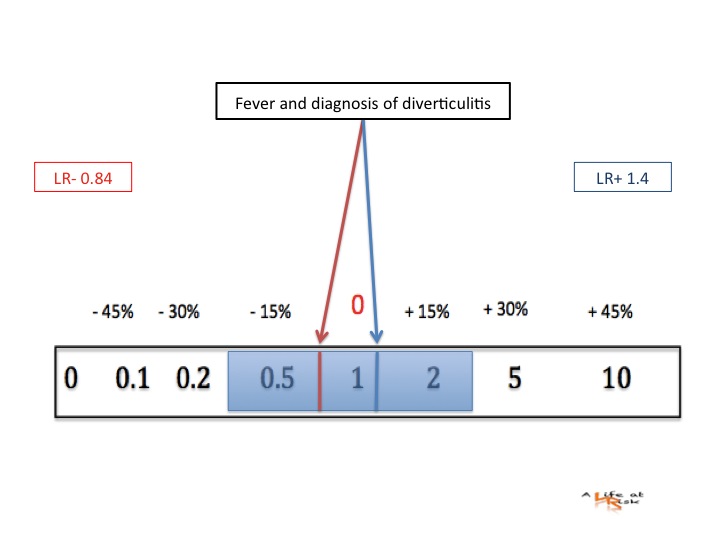
A 66 yo man complains of left lower quadrant (LLQ) abdominal pain from 4/5 hours. The pain is described as crampy initially, than continuous, there is not vomit. Temperature is 37.5°C. Abdomen is treatable, with moderate pain and tenderness localized at LLQ , there is not history of prior abdominal surgery.
Conclusion
The patient presented above has a high probability to have an acute non complicated diverticulitis, imaging tests have a little impact on disease’s management.
Imaging is necessary when all 3 clinical features aren’t present, or when the patient is very ill and the suspect of any complication is very high.
On the other hand the absence of any of 3 clinical features isn’t useful to rule out an acute diverticulitis.
Bibliography
W.Lameris
A clinical decision rule to establish the diagnosis of acute diverticulitis at the Emergency Department.
Dis Colon Rectum 2010 53 896-904
JRT Monson
Management of acute diverticulitis: is less more?
Dis Colon Rectum 2011 54 126-128